1. Lottick EA, inventor; Lottick EA, assignee. Electrocautery hemostat. United States patent US 4,370,980. 1983 Feb 1.
2. Das JM. Bone wax in neurosurgery: a review. World Neurosurg 2018;116:72-76.


3. Horsley V. Antiseptic wax. Br Med J (Clin Res Ed) 1982;1:1165.

4. Parker R. Aural pyaemia successfully treated by removing putrid thrombus of jugular vein and lateral sinus. Br Med J (Clin Res Ed) 1982;1:1076-1077.
5. Sudmann B, Anfinsen OG, Bang G, Koppang R, St├Ėlen SO, Koppang HS, Sudmann E. Assessment in rats of a new bioerodible bone-wax-like polymer. Acta Orthop Scand 1993;64:336-339.


6. Alberius P, Klinge B, Sj├Čgren S. Effects of bone wax on rabbit cranial bone lesions. J Craniomaxillofac Surg 1987;15:63-67.


7. Wellisz T, Armstrong JK, Cambridge J, Fisher TC. Ostene, a new water-soluble bone hemostasis agent. J Craniofac Surg 2006;17:420-425.


8. Low WK, Sim CS. Bone wax foreign body granuloma in the mastoid. ORL J Otorhinolaryngol Relat Spec 2002;64:38-40.


9. Ozdemir N, Gelal MF, Minoglu M, Celik L. Reactive changes of disc space and foreign body granuloma due to bone wax in lumbar spine. Neurol India 2009;57:493-496.


10. Sudmann B, Bang G, Sudmann E. Histologically verified bone wax (beeswax) granuloma after median sternotomy in 17 of 18 autopsy cases. Pathology 2006;38:138-141.


11. Suwanprateeb J, Kiertkrittikhoon S, Kintarak J, Suvannapruk W, Thammarakcharoen F, Rukskul P.
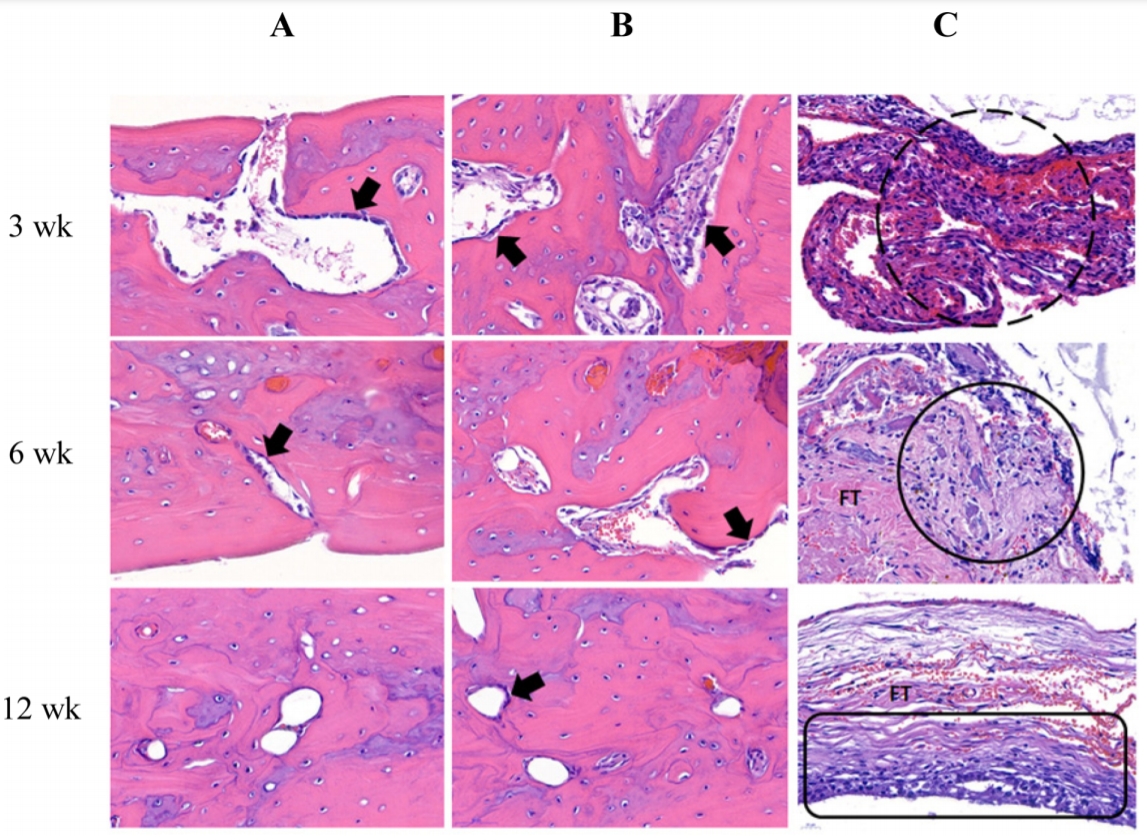
In vivo assessment of new resorbable PEG-PPG-PEG copolymer/starch bone wax in bone healing and tissue reaction of bone defect in rabbit model. J Mater Sci Mater Med 2014;25:2131-2139.


12. Wolvius EB, van der Wal KG. Bone wax as a cause of a foreign body granuloma in a cranial defect: a case report. Int J Oral Maxillofac Surg 2003;32:656-658.


13. Gibbs L, Kakis A, Weinstein P, Conte JE Jr. Bone wax as a risk factor for surgical-site infection following neurospinal surgery. Infect Control Hosp Epidemiol 2004;25:346-348.


14. Angelini GD, el-Ghamari FA, Butchart EG. Poststernotomy pseudo-arthrosis due to foreign body reaction to bone wax. Eur J Cardiothorac Surg 1987;1:129-130.


15. Cirak B, Unal O. Iatrogenic quadriplegia and bone wax. Case illustration. J Neurosurg 2000;92:248.

16. Butterworth J, Douglas-Akinwande A. Lower extremity paralysis after thoracotomy or thoracic epidural: image first, ask questions later. Anesth Analg 2007;104:201-203.


17. Tay HL, Tan LK. Surgical bone wax causing epistaxis. J Laryngol Otol 1996;110:267-268.


18. Chun PK, Virmani R, Mason TE, Johnson F. Bone wax granuloma causing saphenous vein graft thrombosis. Am Heart J 1988;115:1310-1313.


19. Wang MY, Armstrong JK, Fisher TC, Meiselman HJ, McComb GJ, Levy ML. A new, pluronic-based, bone hemostatic agent that does not impair osteogenesis. Neurosurgery 2001;49:962-967.


20. Suwanprateeb J, Suvannapruk W, Thammarakcharoen F, Chokevivat W, Rukskul P. Preparation and characterization of PEG-PPG-PEG copolymer/pregelatinized starch blends for use as resorbable bone hemostatic wax. J Mater Sci Mater Med 2013;24:2881-2888.


22. de Miranda JR, Choi IGG, Moreira MS, Martins MD, Cortes ARG, Yoshimoto M. Histologic evaluation of early bone regeneration treated with simvastatin associated with low-level laser therapy. Int J Oral Maxillofac Implants 2019;34:658-664.


23. Lucaciu O, Gheban D, Soritau O, B─āciu┼Ż M, C├ómpian RS, B─āciu┼Ż G. Comparative assessment of bone regeneration by histometry and a histological scoring system. Rev Rom Med Lab 2015;23:31-45.
24. Ibarrola JL, Bjorenson JE, Austin BP, Gerstein H. Osseous reactions to three hemostatic agents. J Endod 1985;11:75-83.


25. Karabek─▒r HS, Korkmaz S. Residue bone wax simulating spinal tumour: a case report. Turk Neurosurg 2010;20:524-526.

26. Geary JR, Franz VK. New absorbable hemostatic bone wax; experimental and clinical studies. Ann Surg 1950;132:1128-1137.


28. Johnson P, Fromm D. Effects of bone wax on bacterial clearance. Surgery 1981;89:206-209.

29. Kanou M, Ueno T, Kagawa T, Fujii T, Sakata Y, Ishida N, Fukunaga J, Sugahara T. Osteogenic potential of primed periosteum graft in the rat calvarial model. Ann Plast Surg 2005;54:71-78.


30. Seo S, Heo J, Chae J, Jeon S, Kim J, Kang N, Lee K, Kang K. Osteogenic effects on athymic rat calvarial defects by human originated cortical bone. Tissue Eng Regen Med 2009;6:9-14.
31. Orgill DP, Ehret FW, Regan JF, Glowacki J, Mulliken JB. Polyethylene glycol/microfibrillar collagen composite as a new resorbable hemostatic bone wax. J Biomed Mater Res 1998;39:358-363.


32. Schonauer C, Tessitore E, Barbagallo G, Albanese V, Moraci A. The use of local agents: bone wax, gelatin, collagen, oxidized cellulose. Eur Spine J 2004;13 Suppl 1:S89-S96.


33. Short HD. Paraplegia associated with the use of oxidized cellulose in posterolateral thoracotomy incisions. Ann Thorac Surg 1990;50:288-289.


34. Spencer HT, Hsu JT, McDonald DR, Karlin LI. Intraoperative anaphylaxis to gelatin in topical hemostatic agents during anterior spinal fusion: a case report. Spine J 2012;12:e1-e6.

35. Pechar M, Strohalm J, Ulbrich K, Schacht E. Biodegradable drug carriers based on poly(ethylene glycol) block copolymers. Macromol Chem Phys 1997;198:1009-1020.

36. Knop K, Hoogenboom R, Fischer D, Schubert US. Poly (ethylene glycol) in drug delivery: pros and cons as well as potential alternatives. Angew Chem Int Ed Engl 2010;49:6288-6308.


37. Hauet T, Goujon JM, Baumert H, Petit I, Carretier M, Eugene M, Vandewalle A. Polyethylene glycol reduces the inflammatory injury due to cold ischemia/reperfusion in autotransplanted pig kidneys. Kidney Int 2002;62:654-667.













 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



