The application of electrochemotherapy in three dogs with inoperable cancers
Article information
Abstract
Factors such as location, volume, and the type of neoplasm complicate achieving tumor control. Electrochemotherapy (ECT) is a supplementary treatment for inoperable neoplasms in veterinary patients. Three dogs were diagnosed with a tumor. Two were squamous cell carcinoma (SCC), and the other was liposarcoma, each with a single tumor with the size range of 1 to 5 cm. The tumor locations were the cervical, oral, and abdominal cavity. ECT was selected as a treatment. Bleomycin was injected intratumorally at the dose of 0.5 to 1.0 mg/cm3. Five minutes after the injection, electric pulses applied in a sequence of eight pulses lasting 100 µsec each, were delivered in 1,000 V/cm. An evaluation was performed after 1 week, and the next session was administered 2 weeks later. In a patient with oral SCC, the tumor was in partial remission after two sessions of ECT. Another patient with SCC on her neck was showed complete remission after 2 weeks of ECT administration. A third patient showed stable disease for 8 weeks. Complications were mild and transient and included skin necrosis, edema, local pain, and gait disturbance. ECT is a valid adjuvant, especially for inoperable, cutaneous, or accessible intra-abdominal tumors.
Introduction
Cancer remains a significant cause of mortality despite advances in diagnosis and treatment, such as chemotherapy, radiotherapy, and surgical resection. It can be difficult to apply a major treatment because of the site, cost, and the condition of the patient. Research is being conducted on alternative treatment methods for these patients. One alternative treatment being researched is electroporation-based treatments as an adjuvant to chemotherapeutic agents. This biomedical treatment is called electrochemotherapy (ECT) and has been developed into a clinically confirmed treatment for cutaneous and subcutaneous malignant tumors, specifically [1].
ECT is a combination of anticancer drugs with electropermeabilization, which uses electric pulses to permeabilize cell membrane. ECT improves local tumor control without systemic adverse effect. ECT makes it possible to use incompatible medicine topically in drug-sensitive animals [1]. Several cohort studies of animals with spontaneous neoplasm were treated with biphasic electric pulses with specific chemotherapeutic agents like bleomycin and cisplatin [2-10]. Melanoma, squamous cell carcinoma (SCC), various types of sarcoma, and lymphoma have been reported to be successfully treated with ECT in veterinary patients [1].
In veterinary oncology, there are patients with inoperable or obstinate tumors with difficulties such as the lack of marginal space, the location of the lesion, or the recurrence of tumor. Studies that applied ECT to incompletely excised or recurring aponeurotic fibromatosis, sarcomas, and mast cell tumors showed complete or partial remission with low toxicity of the medicine [9-11].
In this study, we describe the application of ECT in three canine patients who were diagnosed cancers, two with SCC and a third with liposarcoma, and evaluate the effectness of ECT on dogs.
Materials and Methods
Samples and patients selection
Between May 2018 and January 2020, 3 privately owned dogs were treated with ECT. The first dog, case 1, was a five-year-old castrated male beagle and referred for cervical masses. The mass rapidly increased over 2 weeks and the patient experienced weight loss. The mass was diagnosed as thyroid carcinoma and SCC and was surgically removed. However, a new mass was found in the cervical area 1 month after surgery.
On physical examination, the patient was bright, active, and alert. The body temperature, pulse, and respiratory rate were in the normal range. The blood pressure of the patient measured 160, which was slightly higher than the average in dogs.
A mass was palpated in the left cervical area. The size of the mass was estimated to be 5.1 cm in diameter. The volume of tumor was calculated to be 62.6 cm3, using the formula ab2π/6. The mass was round and firm. Fine needle aspiration (FNA) was performed. Epithelial cells were the major cells and showed a round to square shape (Fig. 1A). There were many vacuoles around the nucleus, and the proportion of nucleus to the rest of the cell was high. It was tentatively diagnosed with SCC, which was one of the masses removed earlier, and it was regarded as a relapse. Surgery was considered, but it was expected that securing an appropriate surgical margin would be challenging because of the normal anatomical structure of the neck, including the external jugular vein. Surgical removal without clean margins could lead to frequent relapses of cancer. We offered some alternative treatment options and the owner decided to apply ECT.
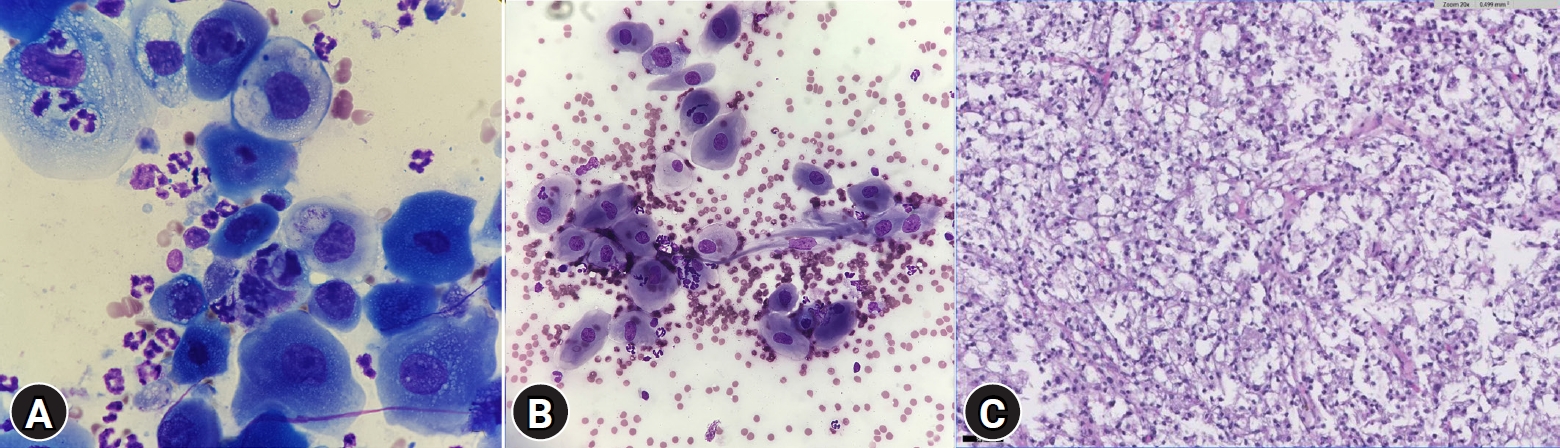
(A) Fine needle aspiration of the cervical mass in case 1. Epithelial cells were major cells and showed round to square shape. Vacuoles are spread throughout the cells (Diff-Quik, ×100 objective). (B) Fine needle aspiration of oral mass in 15-year-old female dog, case 2. Vacuoles are spread throughout the cells. Round to square shaped cells are major type of presenting cells (Diff-Quik, ×100 objective). (C) Histological examination of 10-year-old male dog, case 3. Neoplastic cells contain abundant light basophilic cytoplasm with one or more variably sized discrete intracytoplasmic lipid droplets. The mass was diagnosed as liposarcoma, evaluated grade 1 and its subtype was pleomorphic (×20 objective).
The second dog, case 2, was a 15-year-old female mongrel and referred for an oral mass. She showed loss of appetite, weight loss, and bleeding from the oral mass lesion. The patient was bright, active and alert, and the vital signs were normal on physical examination. The mass was found 3 months prior and the patient had problems closing her mouth because of the mass. The tumor was round and firm, and its size was evaluated as 2.4 cm in diameter. The tumor volume was calculated to be 6.6 cm3, by the formula ab2π/6. The type of tumor was tentatively diagnosed as SCC by FNA (Fig. 1B). Computer tomography was performed, and the tumor was evaluated as invasive to the nasal cavity area and bone lysis was found (Fig. 2). Partial maxillectomy was offered, but the owner refused. Therefore, ECT was chosen as an alternative treatment to improve the patient’s quality of life.
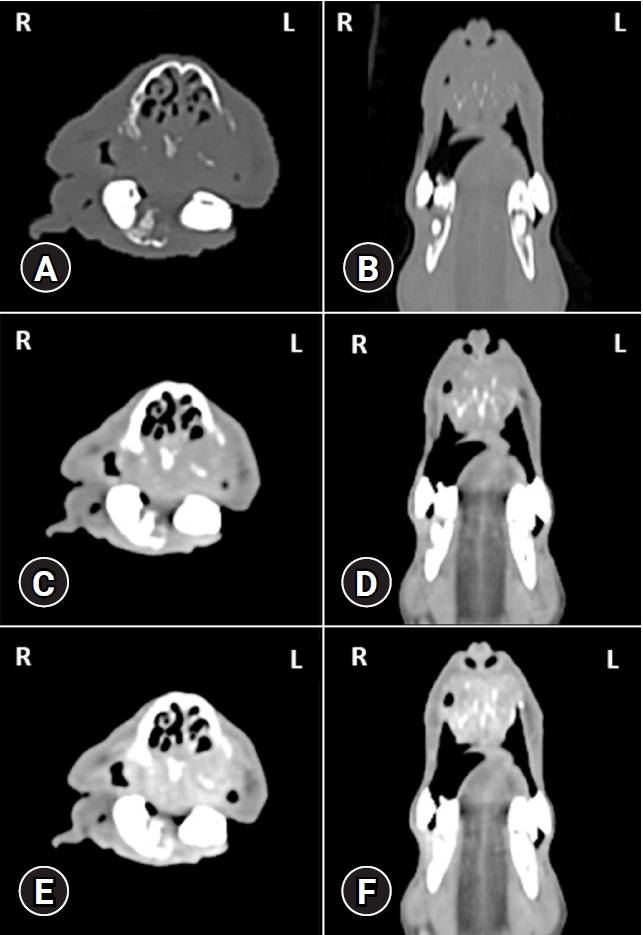
Computer tomography of case 2. The mass was evaluated as invasive to nasal cavity area, lysed the bone. The patient had a problem with chewing. (A) Pre-contrast, bone window, transverse view. (B) Pre-contrast, bone window, dorsal view. (C) Pre-contrast, soft tissue window, transverse view. (D) Pre-contrast, soft tissue window, dorsal view. (E) Post-contrast, delayed phase, transverse view. (F) Post-contrast, delayed phase, dorsal view.
The third dog, case 3, was a 10-year-old castrated male Miniature Pinscher and referred for an abdominal cavity mass. The owner took him to a local animal clinic when he developed vomiting and hematochezia. Ultrasonography and laparotomy were performed, and the mass was found in the abdominal cavity. A biopsy was performed at the same time and the patient was referred to the IDEXX in the hospital.
After the laparotomy and biopsy were performed, the patient was referred to our hospital. He was bright, active, and alert during his physical examination. His vital signs were within the normal range.
On physical examination, the intra-abdominal mass was measured to be 5.6 cm in diameter. When we palpated the mass, it was very firm and round shaped. Ultrasonography was performed, and the mass size was measured at 4.5×4.4×4.1 cm. The volume of mass was calculated to be 42.5 cm3, by the formula abcπ/6. The type of mass was diagnosed as liposarcoma based on histopathology and evaluated grade 1 (Fig. 1C). The mass was attached to abdominal wall and widely diffused to the dorsal side. Thus, a surgical removal would be challenging (Fig. 3).

Computer tomography of case 3. (A) Transverse, pre-contrast. (B) Transverse, post-contrast, artery phase. (C) Transverse, post-contrast, portal phase (D) Transverse, post-contrast, delayed phase. (E) Abdomen, dorsal reconstruction view. (F) Abdomen, sagittal reconstruction view.
Chemotherapy with toceranib at a dose of 2.75 mg/kg on a MWF protocol was initiated and the patient was treated for two months. However, the patient showed no response and the tumor rapidly grew. Three months after the initiation of chemotherapy, the mass could be palpated in the right inguinal region.
Electric chemotherapy protocol
Before treatment, all patients were sedated with a combination of dexmedetomidine (Presedex; Pfizer, Korea), hydromorphone (Dilid Inj.; Hana Pharm, Korea) and ketamine (Ketamine hydrochloride injection; Yuhan, Korea). In case 1, bleomycin (Bleocin inj.; Dong-A ST, Korea) was administered intratumorally after sedation at a dose of 0.5 mg/kg, which is generally consulted maximum dose that would not cause pulmonary toxicity in small animals. In case 2, bleomycin was injected as 0.5 to 1.0 mg/cm3 intratumorally, at a concentration of 3 mg/mL. And after whole ECT sessions were terminated, toceranib was administered at the dose of 2.75 mg/kg on a Monday–Wednesday–Friday (MWF) schedule. In case 3, bleomycin was administered intratumorally at a dose of 0.5 mg/cm3 in the 1st and 2nd session, and 1 mg/cm3 in the 3rd session. Five minutes after the injection of the chemotherapy agent, 8 biphasic pulses were administered to all patients in 0.1 sec intervals, an amplitude of 1,000 V/cm, and at a frequency of 1 Hz.
Results
Treatment response and tolerance
In the first patient, the tumor volume had decreased to 0.29 cm3 after 1 week. After 2 weeks of the session, the tumor was evaluated to be in a complete remission. The patient has remained in complete remission over 10 months.
The second patient was rechecked every week. Six weeks after all ECT sessions were terminated, the tumor volume was reduced to 2.2 cm3. The patient did not show any adverse effect except bleeding from the root of incision teeth, and it disappeared after incision teeth were extracted. Her appetite recovered and body weight was gained. She achieved partial response for about 3 months but was found dead one morning in the owner’s house. The exact cause of death was not identified because necropsy was not performed at the owner’s request. However, we regarded the obstruction of her airway by tumor growth as the major cause of death.
The volume of the tumor of the third patient decreased to 29.8 cm3 after 2 sessions of ECT. However, it increased to 31.9 cm3 after the 3rd session and the patient showed adverse effects like skin necrosis, swelling, and flare of the treated region. The tumor was evaluated as a progressive disease. The skin necrosis was so severe that the ECT sessions were terminated. The patient was evaluated to be in a progressive disease state. The necrotized skin became broader over time, and incrustation started. The patient did not show any pain, but it took about 4 months to be healed. He was bright and very active. After one year, the dog was still alive and the patient’s general condition was well maintained.
Discussion
ECT is being used as an adjuvant treatment of human cutaneous and subcutaneous tumors. There are also veterinary studies that have described the efficacy of ECT in various cutaneous, oral, and inoperable tumors of dogs, cats, and horses [2-12]. Electrical pulses administered to the tumor changes the permeability of the cell membrane. This leads to increased intratumorous concentration of the injected chemotherapy agent leading to cell death. ECT rarely causes systemic adverse effects [13-15]. It is easy to administer and only needs low doses of medicine [16-19].
The anticancer drugs used with ECT are bleomycin, cisplatin, doxorubicin, and mitoxantrone where bleomycin and cisplatin are the most commonly used [15-20]. In the cases described above, bleomycin was ideal as a cytostatic medicine because it is regarded as the cornerstone of ECT and its efficacy is amplified about 700-fold when administered with electropermeabilization. The evaluation of efficacy of electric pulses would be easier than with the other cytotoxic agents [15-18].
In our study, ECT reduced the size of the tumors through all sessions and can be applied repeatedly in case of recurrence. It dramatically reduces tumor size in the first session, but the reduction rate of tumor size decreased gradually while the sessions were repeated. Most cells that are actively dividing are sensitive to the chemotherapeutic agent and affected at the first session, leading to quick cell death. Cells that are not actively dividing and insensitive cells are less affected and remain alive while ECT sessions are being repeated. Moreover, bleomycin is transported by diffusion when injected intratumorally. Bleomycin is a hydrophilic medicine that would not diffuse efficiently nor would be sufficiently transported to cause cell death in cases with large and/or irregular neoplasms. However, more research is needed to understand the exact mechanism of tumor reduction when it is repeatedly applied.
The main side effect is pain in the area where the electrode touches the skin. Some patients have muscle contractions during the treatment. Infection in the area of treatment is rare. An ulcerated, swollen, or painful treatment area with or without discharge, change of skin color are also known as common adverse effects of ECT. In our study, pain and edema of the affected area appeared to be a side effect in all cases. After the procedure, the swelling was relieved by applying an ice pack and disappeared within 3 days. The pain was controlled with tramadol was prescribed at a dose of 2 mg/kg twice a day for 7 days when the patient was in pain after ECT. There is no generally accepted treatment that could prevent or relive the adverse effects of ECT. As general medication about pain and wound, all patients were treated with local lidocaine injection before ECT and ice pack after ECT, but they were not effective to prevent or relieve adverse effect including pain and edema. In case 3, the patient had a severe ulcer in the treated area. The ulcer was located over the entire affected area, and the pain did not seem severe despite widespread ulceration. The ulcer had discharge, which disappeared after two weeks. After months, the ulceration was totally recovered. The patients’ owners were satisfied with the treatment because the pain and edema quickly disappeared and although the ulcer took three months to heal, the patient did not complain of serious discomfort. It can be a great advantage if you apply ECT with proper adjuvant treatment because it has no systemic adverse effects.
To the best of the authors’ knowledge, the third case is the rare example of administering ECT to an intraperitoneal tumor. It was applied with ultrasonography guidance. While ECT was usually very effective in cutaneous or subcutaneous tumor, it did not appear to be curative in an abdominal cavity mass. In cases of a large abdominal mass, only a limited part of the tumor can be approached via cutaneous injection method, unless ECT is performed while the patient is in surgery or laparotomy. Furthermore, even if bleomycin was diluted with 0.9% normal saline in 3 mg/mL as previous studies, the total volume of bleomycin was excessive. It made injecting the total amount of drug to the tumor difficult in cases 1 and 2. In case 3, the tumor had such compacted tissue such that administering medicine was so difficult that we had to apply high pressure to inject drug intratumorously.
In conclusion, ECT is relatively easy to administer, can be performed by veterinarians without specialized training, and shows less systemic adverse effects. Therefore, it is expected to be a choice of alternative therapy that will have an antitumor effect while avoiding systemic adverse effects, particularly when the tumor is sensitive to ECT, such as cutaneous or subcutaneous tumor in dogs.
Notes
The authors declare no conflict of interest.
Acknowledgements
We are thanks to the Cooperative Research Program of Center for Companion Animal Research (Project no. PJ01404502): Rural Development Administration, Republic of Korea for the publication support.
