 |
 |
| Korean J Vet Res > Volume 63(2); 2023 > Article |
|
Abstract
A 10-year-old, spayed female, Maltese dog presented with a 2-day history of severe left eye squint. Slit-lamp biomicroscopy showed a deep corneal defect stained into a doughnut shape together with hypopyon in the anterior chamber. Based on these results, a diagnosis of descemetocele and uveitis in the left eye was made. Deep keratotomy combined with a nictitating membrane flap effectively resolved the descemetocele without complications. The surgical procedures performed on this patient were easy and effective, and could be used as an alternative to graft surgery for descemetocele treatment.
Simple corneal ulcers typically heal within a few days to a week with topical medications, but they can progress rapidly and become deeper, potentially leading to permanent vision loss. In complicated corneal ulcers like descemetocele, surgical interventions are required to promote healing and prevent further complications [1]. Conjunctival grafts have been used for the surgical treatment of complicated corneal ulcers. However, the techniques can be challenging to perform because multiple factors need to be considered during and after surgery. Graft dehiscence accounts for 9% of canine conjunctival grafts [2,3]. On the other hand, superficial keratotomy and/or a nictitating membrane flap (NMF) have been widely used for the surgical treatment of superficial corneal ulcers, but much less frequently for complicated corneal ulcers [4,5]. This report describes the use of deep keratotomy (DK) combined with an NMF to address the descemetocele of a complicated corneal ulcer in a dog.
A 10-year-old, spayed female, Maltese dog presented for ocular evaluation with a 2-day history of severe squinting in the left eye (oculus sinister, OS). The owner reported that the patient was diagnosed with pyometra 7 days prior and was subsequently recovering after ovariohysterectomy. On the first presentation, an apparent deep corneal defect was observed on the axial cornea (Fig. 1A), and mild mucoid discharge and profound blepharospasm were obvious. Menace response, dazzle reflex, and pupillary light reflex were present. Schirmer Tear Test measurement (MSD, USA) was 15 mm/min, and intraocular pressure measurement with rebound tonometry (iCareTonoVet; Tiolat, Finland) was 9 mmHg in the OS. On slit-lamp biomicroscopy of OS (HS-7000; Huvitz Co., Ltd., Korea), marked conjunctival hyperemia with circum-corneal ciliary flush, a deep corneal defect, and corneal mineralization were identified on the anterior ocular surface along with a large amount of cellular infiltration and moderate flare in the anterior chamber (Fig. 1B). The corneal lesion was transparent and oval in shape, and the size of the deeper corneal defect area was 7 mm wide and 5 mm long (Fig. 1). The area of the corneal defect was stained into a doughnut shape along the exposed vertical stromal layer. Fundic examination with indirect ophthalmoscopy (Vantage Plus; Keeler Instruments Inc., USA) was limited due to the corneal conditions, though it appeared normal. The owner did not agree to corneal cytology to identify infectious organisms. Based on the clinical information available, a diagnosis of both descemetocele and anterior uveitis was made.
The conjunctival flap would have been the procedure of choice for the patient to prevent loss of vision. However, surgical options were limited because of financial restrictions and constraints related to anesthetic use arising from ovariohysterectomy performed 7 days previously. Accordingly, topical medications were prescribed as follows: 0.5% moxifloxacin (Vigamox; Alcon Singapore Manufacturing Pte. Ltd., Singapore) and autologous serum every 2 hours. Oral medications comprised doxycycline 5.0 mg/kg twice a day (Doxycycline Hyclate; Kukje Pharm, Korea) and meloxicam 0.1 mg/kg once a day (Meloxifen; Kukje Pharm., Korea). Additionally, commercially available cefazoline powder (Cephazoline Injection 1 g; Chong Kun Dang Pharm, Corp., Korea) for intravenous injection was diluted to prepare a 50 mg/mL (5% cefazoline) solution, which was initiated every 2 hour.
On re-examination 5 days later, the signs of ocular pain such as squinting and ocular discharge were reduced as compared to the first examination, though the depth of the corneal defect appeared to be unchanged. To reduce the time under anesthesia and the financial burden, surgical procedures combining the DK with an NMF were selected. The owner was warned of possible sequelae including vision loss after surgery. There were no remarkable abnormalities in the systemic health conditions for surgery based on routine blood profiles and a radiographic examination. The patient was premedicated with medetomidine (12 μg/kg, Domitor; Pfizer, USA), induced with tiletamine and zolazepam (1.5 mg/kg, Zoletil50; Virbac, France,), and maintained with isoflurane (Ifran; Hana Pharm Co., Korea) and oxygen.
The eye was aseptically prepared with a 0.5% diluted povidone-iodine solution and saline and draped. An eyelid speculum was positioned in the affected eye to secure exposure for the debridement and DK. First, the nonattached epithelial cells and/or necrotic debris on the ulcer bed were debrided with a Swann-Morton 64 microsurgical blade (SM Microsurgical blades, UK). Loose epithelial tissue around the ulcer bed was also removed. Second, deep linear keratotomy was performed using another blade to incise at 1 mm intervals in a radial pattern from the peri-ulcer bed to 2 ± 3 mm beyond the corneoconjunctival limbus. The depth of the keratotomy was less than half the corneal thickness, approximately half of the cutting edge of the blade used (Fig. 2). Lastly, the NMF technique was performed as described previously [5]. Postoperative treatments comprised administering 0.5% moxifloxacin every 8 hours, oral doxycycline 5.0 mg/kg twice a day, and meloxicam 0.1 mg/kg once a day.
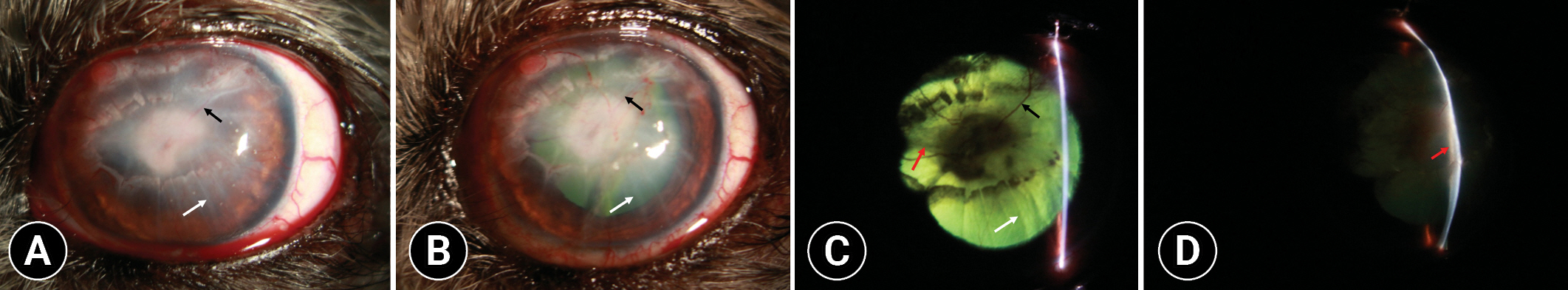
On re-examination, one week postoperatively, the NMF was left in its original place, and no signs of ocular pain were observed when touching the eyelids and the NMF. Oral medications were discontinued and topical treatment was continued at the same dosage frequency for 2 weeks thereafter. Four weeks postoperatively, the NMF was removed. The initial region of the descemetocele was entirely filled with fibrous tissue, in conjunction with several superficial and deep perfused vessels extending from the limbus to the fibrous region (Fig. 3A and B). Marks of radial incisions remained on the corneal surface. Focal corneal granulation tissue was identified in the limbus region at 11 o’clock. There was no positive fluorescein stain uptake except for the granulation tissue area. Several fibrous bands extending from the margin of the pupil to the posterior surface of the fibrous tissue were observed in the anterior chamber (Fig. 3C and D). Topical treatment with 0.1% hyaluronic acid every 4 hours (Hyalon; Samcheondang Pharmaceutical Co., Ltd., Korea) continued for the next 2 weeks. The patient was lost to further follow-up at our clinics. At 5 months postoperatively, telephonic follow-up with the referring veterinarians confirmed no evidence of discomfort in the eye based on the absence of blepharospasm and epiphora with an improvement of the fibrous tissue in the axial cornea.
This report describes the successful surgical treatment of descemetocele using DK combined with an NMF without postoperative complications. This case serves to accentuate the potential for attempting combined surgical interventions on dogs with descemetocele.
The DK was believed to promote the migration of corneal fibroblasts to the ulcer bed through the blood vessels originating from the perilimbal area, leading to the vascular healing of complicated corneal ulcers [3]. The first process of corneal healing is epithelial sliding and mitosis onto the anterior part of the wound, transforming the keratocytes and mononuclear cells into fibroblasts [6]. This plays the important role of a moderator for stromal healing. In addition to that, a complicated corneal ulcer would need a vascular supply from the perilimbal vessels to ensure healing. Superficial keratotomy with involvement up to the basement membrane for the treatment of indolent corneal ulceration serves to facilitate the migration of new epithelial cells and then adherence to the corneal stroma [3]. Thus, the DK used appeared to augment the role of superficial keratotomy in the migration of the corneal epithelium into the ulcer bed. The migrated epithelium from the edge of the injured area over the wound can be protected from the trauma associated with eyelid blinking and rubbing and incorporated with the ulcer bed by the pressure exerted due to the NMF.
Additional injuries to the corneal surface caused by the DK were likely to facilitate corneal healing through higher epithelial migration and proliferation arising from increased expression of heat shock proteins (HSPs) [7]. Of those, HSP70 was thought to be one of the most important HSPs for corneal repair in that it improves the tissue repair through epithelial migration and proliferation [8,9]. These proteins are induced by a variety of environmental stimuli such as trauma, heat shock, and chemical agents. Therefore, this molecular mechanism of corneal healing allows us to postulate that the use of surgical procedures used such as DK appeared to induce these proteins that enhance corneal epithelial healing.
It is generally believed that limbal epithelial stem cells are mainly distributed in the limbal area in dogs [10]. Limbal stem cells proliferated in response to the corneal injury and migrated centripetally, thereby providing renewal of the basal cells and maintaining corneal clarity [11]. On the other hand, several studies have demonstrated that the surgical stimulations in the limbus area and conjunctiva could produce pathological changes in the cornea such as fibrosis and vascularization because of the surgically-induced partial limbal stem cell deficiency [11,12]. Accordingly, the DK could facilitate the migration of the conjunctival vessels onto the corneal ulcer bed, which consequently plays a role similar to that of the fibroblastic tissue and blood vessels in graft surgery (Fig. 3) [8].
In conclusion, the surgical procedures performed in this case are relatively easy, shorten the surgery time, and are low cost compared to conjunctival flaps. This case report suggests a potential for an alternative to graft surgery for the surgical treatment of descemetocele.
Acknowledgments
The author would like to thank Songhui Lee, in the Department of Clinical Sciences, College of Veterinary Medicine and Research Institute for Veterinary Science, Seoul National University, for assistance with illustrations and graphics.
Fig. 1.
Clinical appearance of the left eye on initial presentation. (A) Image by direct diffuse illumination. Note extensive, deep corneal defect with marked conjunctival hyperemia and circum-corneal ciliary flush. (B) Image by direct focal illumination. Note relatively transparent center of corneal ulcer lesion indicating descemetocele and the hypopyon at the anterior chamber indicating uveitis.
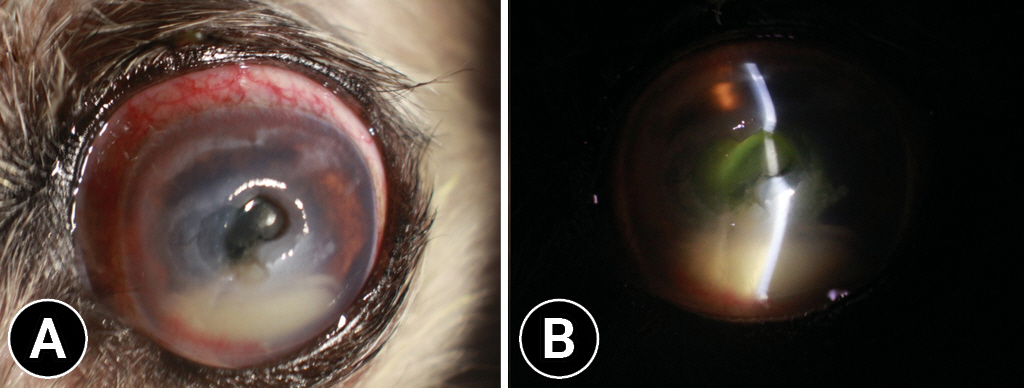
Fig. 2.
Illustration of the surgical procedure for the deep keratotomy. It was performed using a microsurgical blade to incise at 1 mm intervals in a radial pattern from the peri-ulcer bed to 2 ± 3 mm beyond the corneoconjunctival limbus. The depth of the keratotomy was less than half the corneal thickness, approximately half of the cutting edge of the blade used.
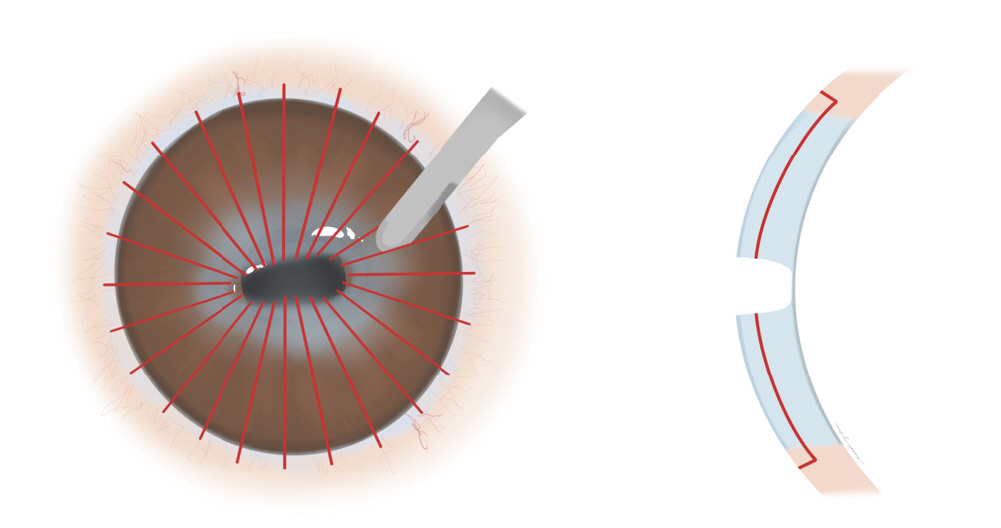
Fig. 3.
Clinical appearance of the left eye immediately following removal of a nictitating membrane flap 28 day after surgery. (A) Image by direct diffuse illumination. Note both the granulated corneal lesion with several intrastromal perfused vessels (black arrow) and a number of deep keratotomies (white arrow) extending from the limbus up to the previous descemetocele area (B) Image by direct diffuse illumination after dilation. The fundus reflex provides better visualization of corneal changes mentioned forehand. (C) Image by focal retroillumination after dilation. Note dyscoria induced by fibrous bands (red arrow) connecting from pupil margin to the posterior surface of corneal lesion. (D) Image by direct focal illumination. Note fibrous membrane (red arrow) covering the posterior corneal surface ulcerated.
References
1. Ledbetter EC, Gilger BC. Diseases and Surgery of the Canine Cornea and Sclera. In: Gelatt KN, Gilger BC, Kern TJ, eds. Veterinary Ophthalmology. 5th ed. pp. 976-1049, Wiley Blackwell, Ames, 2013.
2. Hakanson NE, Merideth RE. Conjunctival pedicle grafting in the treatment of corneal ulcers in the dog and cat. J Am Hosp Assoc 1987;23:641-648.
3. Wilkie DA, Whittaker C. Surgery of the cornea. Vet Clin North Am Small Anim Pract 1997;27:1067-1107.


4. Boutin MP, Coutellier M, Ollivier FJ. Cotton-tip debridement, scalpel blade debridement, and superficial grid keratotomy for treatment of spontaneous chronic corneal epithelial defects (SCCED): a retrospective evaluation of 308 cases. Vet Ophthalmol 2020;23:979-986.



5. Helper LC, Blogg R. A modified third eyelid flap procedure. J Am Anim Hosp Assoc 1983;18:955-956.
6. Maggs D. Corena and Sclera. In: Maggs D, Miller P, Ofri R, eds. Slatter’s Fundamentals of Veterinary Ophthalmology. 5th ed. pp. 184-219, Elsevier, St. Louis, 2013.
7. Kim JM, Kim JC, Park WC, Seo JS, Chang HR. Effect of thermal preconditioning before excimer laser photoablation. J Korean Med Sci 2004;19:437-446.



8. Zhang J, Huang C, Feng Y, Li Y, Wang W. Comparison of beneficial factors for corneal wound-healing of rat mesenchymal stem cells and corneal limbal stem cells on the xenogeneic acellular corneal matrix in vitro. Mol Vis 2012;18:161-173.


9. Peterson CW, Carter RT, Bentley E, Murphy CJ, Chandler HL. Heat-shock protein expression in canine corneal wound healing. Vet Ophthalmol 2016;19:262-266.


10. Morita M, Fujita N, Takahashi A, Nam ER, Yui S, Chung CS, Kawahara N, Lin HY, Tsuzuki K, Nakagawa T, Nishimura R. Evaluation of ABCG2 and p63 expression in canine cornea and cultivated corneal epithelial cells. Vet Ophthalmol 2015;18:59-68.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,882 View
- 62 Download
- ORCID iDs
-
Manbok Jeong

https://orcid.org/0000-0002-0155-1109 - Related articles

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



