Broncholithiasis is defined as the presence of mineralized material within the bronchial lumen [
1]. In humans, broncholithiasis is a rare disorder with an incidence of 0.1% to 0.2% of all lung diseases [
2]. In humans, the most common cause of broncholithiasis is erosion of the bronchial lumen by calcified adjacent lymph nodes and extrusion of calcified adjacent lymph nodes into bronchial the lumen, usually associated with tuberculosis or histoplasmosis [
3]. The presence of broncholithiasis suggests a chronic time course of airway inflammation in cats [
4]. This condition has not been reported in dogs [
5].
Thoracic radiography shows mineralized opacity embedded in the intraluminal bronchial material of soft tissue opacity [
4,
6]. Interstitial patterns can be identified in the lung lobe surrounding the lesion [
4]. When these findings are confirmed by radiographic imaging, differential diagnoses include broncholithiasis, bronchopulmonary tumor with calcification, asthma, chronic bronchitis, and pulmonary alveolar microlithiasis (PAM) [
6]. Definitive diagnosis can be established on thoracic computed tomography (CT) to identify the presence of features of chronic inflammatory airway disease and the location of mineralized material within the bronchial lumen [
4].
To our knowledge, only 5 cases of broncholithiasis in cats have been reported in the veterinary literature [
3,
5-
7]. However, only one case described the CT appearance of broncholithiasis in cats [
4]. The purpose of this study was to describe the CT features of broncholithiasis with bronchitis in a cat.
A 5-year-old castrated male, domestic shorthair cat was referred for further investigation of pulmonary nodules that were incidentally detected on thoracic radiographs for health screening. On physical examination, the cat weighed 8.0 kg and the body condition score was 8 out of 9. Tachypnea (102 breaths per minute) with a normal respiratory pattern most likely due to anxiety and clear lung sounds were confirmed on pulmonary auscultation. Heart rate and temperature were normal. Complete blood count and biochemistry were unremarkable except for mild hyperglobulinemia (5.2 g/dL; reference range, 2.5-4.5 g/dL).
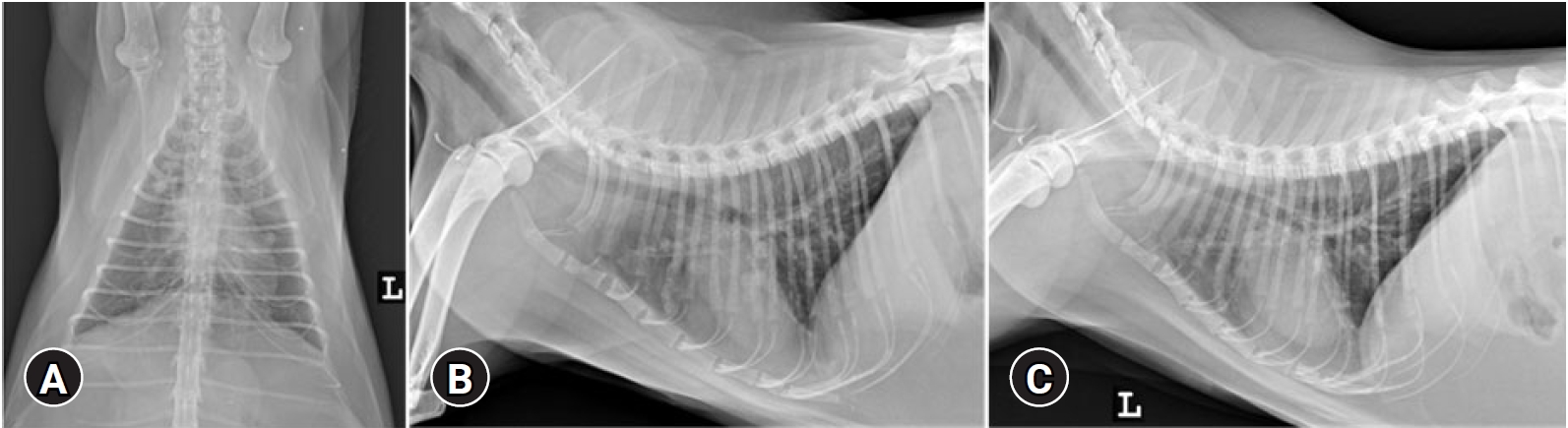
Thoracic radiographs (54 kVp, 400 mA, 6.3 mAs; Regius model 190; KONICA Minolta, Japan) identified ill-defined nodular or tubular-shaped soft tissue opacity lesions throughout all pulmonary lobes, but these lesions were more severe in bilateral cranial lung lobes. Soft tissue opacity lesions in bilateral cranial lobes and the right caudal lung lobe were characterized by the presence of multiple faint mineral opacities (
Fig. 1). A mild bronchointerstitial pattern was identified in all pulmonary lobes. Thoracic CT was performed under general anesthesia using contiguous 0.5 mm helical slices (Aquilion Lightning 160; Canon Medical Systems, Japan). The scanning parameters of the CT were as follows: 120 kVp, 100 mAs, 1 mm collimation, 0.75 seconds rotation time, and pitch factor of 1.475. The CT scan was performed in the sternal recumbency at the end-inspiration. End-inspiration was induced by manually compressing the reservoir bag of the anesthetic machine to achieve an airway pressure of 15 cmH
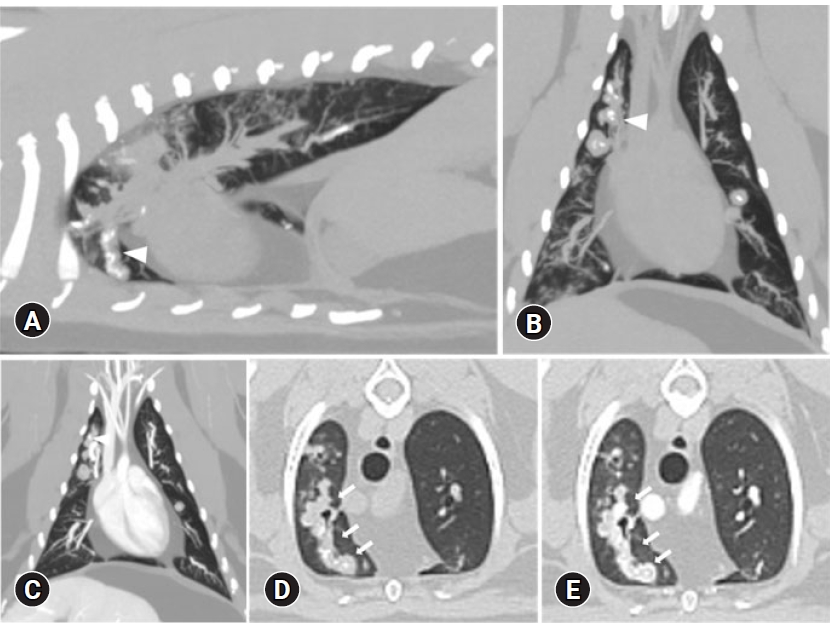
2O. Multiplanar reconstructions as well as maximal intensity projection reconstructions (
Fig. 2) and minimal intensity projection reconstructions were performed. Bronchial dilation and bronchial wall thickening were identified in the bilateral cranial and accessory lung lobes. Round to ellipsoid mineralized concretions measuring 1 to 2 mm in diameter were found embedded in the intrabronchial soft tissue opacity material in bilateral cranial and accessory lung lobes. Concretions were too small to accurately assess the opacity, but they ranged from 700 to 1,300 HU. There was minimal to no enhancement after contrast administration. Hyperinflation was identified in the right cranial lung lobe, caudal part of the left cranial lung lobe, and accessory lung lobe, which was considered to be caused by bronchial obstruction. The hyperinflated lung lobes were identified to have reduced attenuation compared to the other lung lobes. The HU value of the hyperinflated lung lobe (-900 to -1,000 HU) was lower than that of other lobes (-600 to -700 HU). Focal ground glass opacity was found in the dorsal aspect of the right cranial lung lobe. A parenchymal band and subpleural band were identified in the right caudal lung lobe. Peripheral poorly-defined, small centrilobular soft tissue attenuation nodules were connected to linear branching structures (a tree-in-bud pattern).
A tracheal wash was performed. On cytological analysis of tracheal wash fluid, at least 70% macrophages, 24% eosinophils, few neutrophils, and normal epithelial cells were found. No microorganisms were identified. Based on radiography, CT, and cytology, the disease condition was tentatively diagnosed as broncholithiasis with bronchitis. The cat was not prescribed any medications. After the 3-month follow-up, no clinical sign associated with pulmonary disease was detected. Thoracic radiography and CT examination was performed, and significant changes were not identified.
Broncholithiasis is defined as a condition in which ossified or calcified material is present in the bronchial lumen [
3]. It is a rare sequel to inflammatory bronchial disease [
8]. Clinical findings of broncholithiasis in cats include hyporexia, weight loss, lethargy, cough, and dyspnea; and respiratory symptoms may not develop in cats [
4-
6]. Clinical relevance may be low if broncholithiasis is found incidentally in cats with no specific lower respiratory tract sign on physical examination [
4].
Thoracic radiography shows small mineralized opacities scattered throughout the lung fields present within the bronchi [
8]. Atelectasis of obstructed lobes/areas and hyperinflation may be seen [
8]. Thoracic CT was performed in only 2 cases of feline broncholithiasis, and mineralized endobronchial concretions were found embedded in the intraluminal soft tissue opacity bronchial material [
4]. In our case, a respiratory sign was absent and radiographs revealed multifocal ill-defined, nodular or tubular soft tissue opacities with internal faint mineral opacity. Primary lung tumor with dystrophic mineralization, PAM, and broncholithiasis were considered as differential diagnoses.
PAM is a very rare condition [
9]. In veterinary literature, reports of this disease in dogs [
9,
10] and a cat [
7] have been presented. Radiographic appearance of PAM in a cat was reported in only one case, which showed multifocal patchy alveolar infiltrates in all lung lobes but miliary mineral opacity was not observed [
7]. On necropsy, round to irregular shaped microliths were found scattered throughout all lung lobes [
7]. In humans, pathognomonic grainy alveolar mineral opacities were identified by thoracic radiography [
11]. In dogs, a pulmonary miliary pattern associated with mineralization has been revealed in thoracic radiographs [
9,
10,
12]. Considering the previous cases, microliths were distributed throughout the lung lobe in PAM patients. In our case, broncholiths were located within round to tubular soft tissue opacities and some of them were distributed linearly. Therefore, the possibility of PAM was judged to be low, but a CT scan was needed to accurately evaluate it.
The radiographic findings of lung tumors in cats vary widely [
13,
14]. The most common primary lung tumors in cats are adenocarcinoma, squamous cell carcinoma, and bronchoalveolar carcinoma [
15]. Any type of a tumor can present with a solitary pulmonary nodule or multifocal pulmonary nodules [
13,
14]. These tumors are often cavitated or partially mineralized [
14]. Since these findings were similar to the radiographic findings of our case, additional CT examination was required for differentiation. On CT examination, the most frequent imaging feature of tumors was a well-defined mass with an irregular margin [
14]. Also, heterogeneous contrast enhancement may be seen [
14]. Many of the tumors may be associated with bronchial compression [
14]. In our case, CT revealed that mineral attenuation material was embedded in the endobronchial soft tissue attenuating material. However, there was minimal to no contrast enhancement. Therefore, the possibility of a tumor was considered to be low and it was tentatively diagnosed as broncholithiasis.
In previously reported cases, CT scans of only 2 cats with broncholithiasis showed that mineralized endobronchial concretions were found embedded in intraluminal soft tissue attenuating bronchial material and bronchiectasis and bronchial wall thickening were also observed [
4]. These findings were similar to those in our case. However, the distribution of broncholithiasis was slightly different. In the previous cases, broncholiths were found in the right middle lung lobe, both caudal lung lobes, and left caudal lung lobe [
4]. In our case, broncholiths were found in both the cranial lung lobe and accessory lung lobe. Therefore, it was thought that broncholithiasis may occur in the bronchus of any lung lobe.
A limitation of this study was that calcification of the pulmonary vascular wall could not be excluded because biopsy was not performed. However, in the arterial phase of thoracic CT, contrast enhancement of the lesions was not confirmed, so it could be diagnosed as broncholithiasis. Another limitation was not perform bronchoalveolar lavage (BAL) and bacterial culture. Although tracheal wash was performed instead of BAL, it is difficult to accurately diagnose bronchus lesions.
This report described the CT diagnosis of broncholithiasis, which has been rarely reported in a cat. On thoracic radiography, broncholithiasis should be considered if mineral opacity lesions are identified in the lung field with evidence of chronic bronchial disease, especially when they are linearly arranged, even if there are no respiratory symptoms. CT scan would be useful in diagnosing broncholithiasis.














 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



